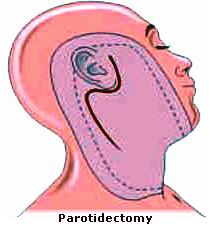
Parotidectomy is a surgical procedure performed to remove part or all of the parotid glands, the largest salivary glands located on either side of the face, in front of the ears. These glands are responsible for producing saliva, which aids in digestion and keeps the mouth moist. Parotidectomy is primarily performed when there are tumors or other abnormalities in the parotid glands, although it may also be done to treat other conditions such as chronic infections or certain types of salivary gland diseases.
This surgery can be necessary when the parotid gland becomes swollen due to tumors (benign or malignant), blockages, or infections. Tumors in the parotid gland can range from non-cancerous (benign) to cancerous (malignant), and their removal is often vital for preventing the spread of cancer or alleviating symptoms caused by benign tumors.
Parotidectomy can be performed using different techniques depending on the location and size of the tumor, as well as whether it is benign or malignant. The most common types of parotidectomy include superficial parotidectomy, total parotidectomy, and modified radical parotidectomy.
While parotidectomy is an effective treatment, it requires careful surgical planning due to the delicate nature of the area. The proximity of critical structures like the facial nerve, blood vessels, and ear makes the procedure complex. Therefore, the surgeon must take great care to avoid damage to these structures during surgery.
The need for a parotidectomy arises from a variety of causes, most commonly related to tumors or infections in the parotid glands. The decision to undergo surgery depends on the cause of the condition and whether it is affecting other structures in the body.
Common Causes for Parotidectomy:
-
Benign Tumors:
-
The most common reason for parotidectomy is the removal of benign (non-cancerous) tumors, such as:
-
Pleomorphic adenoma: A slow-growing benign tumor that is the most common type of salivary gland tumor. These are usually located in the superficial part of the parotid gland and are often painless.
-
Warthin’s tumor: A benign tumor that typically affects older adults, especially male smokers. It usually appears in the lower part of the parotid gland.
-
Monomorphic adenoma: Another type of benign tumor, rarer than pleomorphic adenomas, often requiring surgical removal.
-
-
-
Malignant Tumors:
-
Though less common, malignant tumors (cancerous tumors) of the parotid gland are serious and often require total parotidectomy (removal of the entire gland) to prevent the spread of cancer. Malignant tumors may include:
-
Mucoepidermoid carcinoma: A cancer that starts in the salivary glands and can be either low-grade (slow-growing) or high-grade (aggressive).
-
Adenoid cystic carcinoma: A rare but aggressive type of cancer that often spreads to other parts of the body.
-
Acinic cell carcinoma: A cancer that occurs in the parotid gland, commonly affecting younger patients.
-
-
-
Chronic Infections:
-
Chronic or recurrent infections in the parotid glands, known as sialadenitis, can lead to the need for surgery, particularly if the infection is not responsive to antibiotics or results in complications like abscess formation.
-
-
Salivary Duct Stones (Sialolithiasis):
-
Salivary stones are calcified deposits that block the ducts of the parotid glands, leading to pain, swelling, and difficulty in saliva flow. If conservative treatments fail, parotidectomy may be required to remove the affected gland or part of it.
-
-
Congenital Abnormalities:
-
Some individuals are born with congenital abnormalities of the parotid glands, which may lead to the need for surgical correction.
-
-
Salivary Gland Cysts:
-
Cysts can form in the parotid glands and, although typically benign, may cause discomfort, infections, or cosmetic concerns, necessitating removal.
-
Risk Factors for Parotid Gland Diseases:
-
Age:
-
Tumors of the parotid gland are more commonly diagnosed in adults, particularly in individuals aged 50-70. However, salivary gland tumors can occur in any age group.
-
-
Smoking:
-
Smoking is a major risk factor for the development of Warthin’s tumors, a benign condition that affects the parotid gland more commonly in men, particularly those who smoke.
-
-
Radiation Exposure:
-
Previous radiation therapy to the head and neck region, especially during childhood, increases the risk of developing tumors in the parotid glands. This is a significant risk factor for both benign and malignant parotid tumors.
-
-
Genetics:
-
Family history plays a role in the development of certain types of parotid gland conditions, especially malignant tumors. Genetic syndromes such as von Recklinghausen’s disease or MEN1 may predispose individuals to salivary gland cancers.
-
-
Gender:
-
Some salivary gland conditions, like Warthin’s tumors, are more common in men. Other conditions, such as pleomorphic adenomas, occur in both men and women.
-
The symptoms that prompt the need for parotidectomy typically arise from abnormal growths, infections, or blockages in the parotid glands. Early detection of these symptoms can lead to more effective treatment and better outcomes.
Common Symptoms of Parotid Gland Disorders:
-
Painless Lump or Swelling:
-
The most common symptom of parotid gland tumors is the development of a painless lump or swelling near the jawline or just in front of the ear. This lump may vary in size and can be felt under the skin.
-
-
Pain or Tenderness:
-
In some cases, parotid tumors or infections may cause pain or tenderness in the affected area, especially when chewing, swallowing, or talking.
-
-
Dry Mouth:
-
A blockage in the parotid duct or chronic inflammation may result in reduced saliva production, leading to a sensation of a dry mouth. This can also make swallowing and speaking difficult.
-
-
Facial Weakness or Numbness:
-
Because the facial nerve runs through the parotid gland, a tumor or infection near the facial nerve may lead to facial weakness, numbness, or asymmetry in the face. This is a serious symptom that requires immediate medical evaluation.
-
-
Difficulty Swallowing:
-
When the parotid gland becomes enlarged or infected, it can press on the throat or other parts of the head and neck, causing difficulty swallowing or a feeling of something being stuck in the throat.
-
-
Fever and Swelling:
-
In cases of infection (sialadenitis) in the parotid gland, patients may experience fever, swelling, and redness in the affected area. Pus or drainage may also be seen in some cases.
-
Diagnosing a condition that requires parotidectomy involves a series of steps to identify the exact cause of the parotid gland abnormalities. A combination of medical history, physical examinations, imaging studies, and biopsies are used to accurately diagnose the condition.
Diagnostic Methods:
-
Physical Examination:
-
The physician will examine the parotid gland for swelling, tenderness, or lumps. They will also check for signs of infection, facial nerve involvement, or other abnormalities.
-
-
Imaging Studies:
-
Ultrasound: An ultrasound is often the first imaging test to evaluate the parotid gland. It can help determine whether the mass is solid or cystic and whether it is benign or suspicious for cancer.
-
CT Scan: A CT scan provides detailed cross-sectional images and is often used for larger tumors or when more information is needed to determine the exact location and extent of the tumor.
-
MRI: An MRI may be used to get detailed images of the parotid gland and surrounding structures, especially when the facial nerve is involved.
-
-
Fine Needle Aspiration (FNA):
-
FNA biopsy is a procedure where a fine needle is used to extract a small sample of tissue from the parotid tumor. This sample is examined under a microscope to check for cancerous cells.
-
-
Excisional Biopsy:
-
In some cases, if FNA results are inconclusive, an excisional biopsy is performed. This involves surgically removing part of the tumor for further examination.
-
The treatment of conditions requiring parotidectomy depends on the nature of the problem—whether it’s a benign tumor, malignant tumor, or infection. Surgical removal of the parotid gland or part of it is the primary treatment.
Surgical Options:
-
Superficial Parotidectomy:
-
In superficial parotidectomy, the outer portion of the parotid gland is removed. This procedure is often used for benign tumors located in the outer part of the gland. It typically involves less risk of facial nerve injury.
-
-
Total Parotidectomy:
-
If the tumor is malignant or if the entire gland needs to be removed, total parotidectomy is performed. This surgery involves removing the entire parotid gland and may require the removal of lymph nodes and surrounding tissue as well.
-
-
Modified Radical Parotidectomy:
-
For more aggressive tumors, a modified radical parotidectomy involves the removal of both the parotid gland and some of the nearby lymph nodes.
-
-
Facial Nerve Preservation:
-
One of the main concerns during parotidectomy is preserving the facial nerve, which controls facial expression. Surgeons use advanced techniques to identify and protect the facial nerve during the procedure.
-
Non-Surgical Options:
-
Antibiotics:
-
If an infection is present, antibiotics may be prescribed to treat the infection and reduce inflammation. If an abscess is formed, drainage may be necessary.
-
-
Radiation Therapy:
-
If a malignant tumor is removed, radiation therapy may be recommended after surgery to target any remaining cancer cells and reduce the risk of recurrence.
-
-
Chemotherapy:
-
For advanced or metastatic parotid cancer, chemotherapy may be used in conjunction with surgery and radiation therapy.
-
While it’s difficult to prevent tumors or other conditions of the parotid glands, maintaining overall health can help reduce the risk of parotid gland disorders.
Prevention:
-
Avoid Smoking:
-
Smoking is a significant risk factor for developing Warthin’s tumor, a benign parotid gland tumor. Quitting smoking can help reduce the risk of these tumors.
-
-
Limit Radiation Exposure:
-
Avoid unnecessary radiation treatments to the head and neck area, especially in children, as this increases the risk of salivary gland tumors later in life.
-
-
Maintain Good Oral Hygiene:
-
Proper oral care, hydration, and managing oral infections can help prevent salivary gland infections.
-
Post-Surgical Management:
-
Follow-Up Care:
-
After parotidectomy, regular follow-up appointments are important to monitor for signs of infection, recurrence of the tumor, and any complications such as facial nerve weakness.
-
-
Physical Therapy:
-
If the facial nerve is affected during surgery, physical therapy may help restore facial muscle strength and prevent long-term facial asymmetry.
-
-
Lymphedema Management:
-
For patients who undergo lymph node removal during surgery, managing lymphedema (swelling) with massage, compression garments, and exercises is crucial.
-
As with any surgery, parotidectomy carries risks and potential complications, which may include:
-
Infection:
-
Infection at the surgical site is a risk, and patients should follow wound care instructions to minimize this risk.
-
-
Facial Nerve Damage:
-
The facial nerve, which runs through the parotid gland, is at risk during surgery. Damage to the facial nerve can result in temporary or permanent facial weakness or paralysis.
-
-
Lymphedema:
-
Removal of lymph nodes can lead to swelling, particularly in the face or neck area, which may require ongoing management.
-
-
Scarring:
-
Although surgeons aim to minimize visible scarring, some scarring may be inevitable, especially for larger tumors or more extensive surgeries.
-
-
Recurrence of Tumors:
-
There is always a risk that the tumor may recur after surgery, particularly in cases of malignant tumors.
-
After parotidectomy, many patients are able to return to their normal activities with the proper care. However, the recovery process varies depending on the extent of the surgery, the type of tumor, and whether additional treatments such as radiation therapy are required.
Recovery and Lifestyle Adjustments:
-
Wound Care:
-
Proper care of the surgical site is essential to avoid infection and promote healing. Follow the instructions provided by the surgeon to care for the incision area.
-
-
Physical Therapy:
-
In cases where facial nerve damage occurs, rehabilitation exercises can help restore normal movement and symmetry. Physical therapy can also be used to manage swelling if lymphedema develops.
-
-
Diet and Oral Care:
-
Since the parotid glands play a role in saliva production, patients may experience dry mouth after surgery. Drinking plenty of fluids and using saliva substitutes can help manage this.
-
1. What is a parotidectomy?
A parotidectomy is a surgical procedure in which part or all of the parotid gland, the largest salivary gland located near the jaw and in front of the ear, is removed. This surgery is typically performed to treat conditions such as benign or malignant tumors, infections, or other disorders affecting the parotid gland.
2. Why would I need a parotidectomy?
Parotidectomy is usually recommended when there is a growth or tumor in the parotid gland, which could be benign (non-cancerous) or malignant (cancerous). It may also be performed if the gland is affected by infections, abscesses, or other conditions that do not respond to other treatments. Removal of the gland or tumor may be necessary to prevent the spread of cancer or to alleviate symptoms caused by the growth.
3. What are the different types of parotidectomy?
There are several types of parotidectomy, depending on how much of the gland needs to be removed:
-
Superficial parotidectomy: Removal of only the outer portion of the parotid gland, leaving the deeper parts intact.
-
Total parotidectomy: Removal of the entire parotid gland, including the deeper portions.
-
Selective parotidectomy: Removal of specific areas of the gland, typically when a tumor is localized in a particular region.
4. How is a parotidectomy performed?
Parotidectomy is usually performed under general anesthesia. The surgeon makes an incision near the ear or along the jawline, carefully dissects through the tissue to access the parotid gland, and then removes the affected portion or the entire gland. If a tumor is present, it will be excised, and care is taken to avoid damaging the facial nerve, which runs through the gland.
5. What are the risks and complications of parotidectomy?
Like any surgical procedure, parotidectomy carries risks, including infection, bleeding, scarring, and adverse reactions to anesthesia. A significant risk is damage to the facial nerve, which can result in facial weakness or paralysis. While rare, it is possible for the tumor to recur or for complications to arise related to the healing of the salivary duct.
6. What is the recovery process after a parotidectomy?
After parotidectomy, most patients stay in the hospital for 1 to 2 days for monitoring. Swelling and bruising around the surgical site are common in the first few weeks. Patients may need to avoid strenuous activities, bending over, or lifting heavy objects for a few weeks to allow proper healing. Most people can return to their normal activities in about 2 to 4 weeks, but full recovery may take several months, especially if the facial nerve is involved.
7. Will I experience facial nerve damage after parotidectomy?
One of the major risks of parotidectomy is damage to the facial nerve, which controls the muscles of the face. While modern surgical techniques aim to minimize this risk, some temporary weakness or drooping of the face may occur after surgery. In most cases, this improves with time, but in rare instances, permanent facial nerve damage may result. Your surgeon will take extra care to preserve the facial nerve during the procedure.
8. What should I expect during the recovery period after parotidectomy?
During recovery, you may experience swelling, pain, or tightness around the surgical site, which can be managed with pain medications. A drain may be placed near the incision site to prevent fluid buildup. It is important to follow your doctor's instructions on caring for the wound and to avoid activities that may put stress on the area, such as heavy lifting or vigorous exercise. Regular follow-up visits are necessary to monitor healing and detect any complications.
9. Are there any lifestyle changes needed after parotidectomy?
After surgery, most patients can return to their normal diet and daily activities once recovery has progressed. However, you may need to make some temporary adjustments, such as avoiding spicy or acidic foods that could irritate the surgical site, especially if you have any dry mouth or difficulty swallowing. For patients who have facial nerve involvement, physical therapy or facial exercises may be recommended to improve facial muscle strength and coordination.
10. What happens if the tumor is malignant (cancerous)?
If the tumor removed from the parotid gland is found to be malignant (cancerous), additional treatments such as radiation therapy, chemotherapy, or further surgery may be recommended, depending on the stage of the cancer and the extent of the tumor. Your oncologist will discuss a personalized treatment plan to ensure the best possible outcome and prevent the cancer from spreading.
The other general procedures are:
Few Major Hospitals for Parotidectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Parotidectomy | Hospitals Parotidectomy | Doctors Parotidectomy | Surgery Parotidectomy | Cost Of Parotidectomy | Treatment For Parotidectomy | Destinations For Parotidectomy | Risks Parotidectomy | Parotidectomy India | Parotidectomy Recovery | Parotidectomy Information | Parotidectomy Thailand | Parotidectomy Malaysia | Parotidectomy Abroad | Parotidectomy Overseas | Parotidectomy Low Cost | Parotidectomy Singapore | Parotid Gland | Salivary Gland | Tumor | Masseter Muscle | Tumors Of Parotid Gland | Total Parotidectomy | Mastoid | Superficial Parotidectomy
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



