A pancreas transplant is a surgical procedure in which a diseased or non-functioning pancreas is replaced with a healthy pancreas from a donor. The pancreas is an essential organ that plays a key role in regulating blood sugar levels and producing digestive enzymes. A pancreas transplant is typically performed on individuals with type 1 diabetes, a condition in which the immune system attacks and destroys the insulin-producing beta cells of the pancreas, leading to chronic high blood sugar levels and, in many cases, complications like kidney failure.
The goal of a pancreas transplant is to restore normal insulin production, control blood sugar levels, and improve the patient’s quality of life. For patients with end-stage diabetes or those with diabetic complications, this procedure can offer a more permanent solution compared to insulin therapy or lifestyle management. In some cases, a pancreas transplant is performed in combination with a kidney transplant if the patient also suffers from diabetic nephropathy (kidney disease caused by diabetes).
A pancreas transplant is typically considered for individuals with poorly controlled blood sugar levels, severe complications from diabetes, or those who are unable to maintain blood sugar control through other means. The transplant procedure, while highly successful for many, carries risks such as rejection, infection, and the need for lifelong immunosuppressive medications to prevent the body from rejecting the transplanted organ.
A pancreas transplant is usually performed in patients with type 1 diabetes, though it can also be considered for individuals with type 2 diabetes in specific cases. The need for a pancreas transplant arises from the pancreas's inability to produce insulin, resulting in poor blood sugar control and an increased risk of complications. Here are the most common causes and risk factors for requiring a pancreas transplant:
1. Type 1 Diabetes
Type 1 diabetes is an autoimmune disorder where the body's immune system mistakenly attacks and destroys the insulin-producing beta cells of the pancreas. Over time, individuals with type 1 diabetes require insulin therapy to regulate their blood sugar levels. A pancreas transplant can restore insulin production and eliminate the need for insulin injections. Type 1 diabetes is the primary condition for pancreas transplants, especially for those with poor blood sugar control or severe complications.
2. Diabetic Nephropathy
Diabetic nephropathy, or kidney disease caused by diabetes, is a common complication of type 1 diabetes and may eventually lead to kidney failure. In these cases, a combined pancreas and kidney transplant may be performed to address both organ failures simultaneously. A functioning pancreas can improve kidney function and overall health by eliminating the need for insulin therapy, which is often a burden for people with diabetic kidney disease.
3. Inadequate Blood Sugar Control
For some individuals with diabetes, managing blood sugar levels with insulin therapy may become increasingly difficult due to complications such as hypoglycemia unawareness (an inability to recognize low blood sugar) or severe blood sugar fluctuations. If blood sugar levels cannot be adequately controlled with insulin therapy, a pancreas transplant may be an option to restore normal glucose regulation.
4. Complications from Type 1 Diabetes
Long-term, poorly controlled diabetes can lead to severe complications such as:
-
Diabetic retinopathy (damage to the eyes)
-
Cardiovascular disease
-
Neuropathy (nerve damage)
-
Amputations
A pancreas transplant can provide significant relief from these complications and improve the patient's overall health and quality of life.
5. Type 2 Diabetes (In Specific Cases)
Although pancreas transplants are more commonly performed for patients with type 1 diabetes, it may also be considered for certain patients with type 2 diabetes. Typically, these patients are individuals who have severe complications, have not responded well to other treatments, or have insulin-dependent diabetes combined with kidney failure.
The symptoms that lead to the need for a pancreas transplant are often related to poor blood sugar control and the complications of diabetes. Some of the most common symptoms and signs that may indicate a pancreas transplant is necessary include:
1. Uncontrolled Blood Sugar Levels
Patients with type 1 diabetes often experience fluctuating blood sugar levels despite insulin therapy. High blood sugar (hyperglycemia) and low blood sugar (hypoglycemia) can be difficult to manage, leading to discomfort, complications, and long-term damage to organs. This lack of control often prompts the consideration of a pancreas transplant.
2. Severe Hypoglycemia
Severe hypoglycemia or low blood sugar is a life-threatening complication of diabetes. Symptoms may include dizziness, confusion, fainting, or seizures. Over time, hypoglycemia unawareness can develop, making it difficult for individuals to recognize when their blood sugar is dangerously low. A pancreas transplant can help prevent these episodes by restoring insulin production.
3. Frequent Urination and Excessive Thirst
Inadequately controlled blood sugar can cause frequent urination (polyuria) and excessive thirst (polydipsia), as the kidneys work harder to filter excess sugar from the bloodstream. These symptoms can significantly impact a patient’s quality of life and may indicate the need for a pancreas transplant.
4. Fatigue and Weakness
Chronic high blood sugar can cause fatigue, weakness, and a general lack of energy. These symptoms often worsen as diabetes progresses and the pancreas's ability to regulate insulin diminishes. A pancreas transplant can improve energy levels and overall vitality.
5. Nerve Damage (Neuropathy)
Chronic high blood sugar can lead to nerve damage, known as diabetic neuropathy, which may cause pain, numbness, tingling, or weakness, especially in the hands and feet. This is a sign that diabetes is affecting other parts of the body and may lead to the need for a pancreas transplant.
6. Vision Problems
People with uncontrolled diabetes are at risk for developing diabetic retinopathy, which can lead to vision problems or even blindness. A pancreas transplant may help prevent or alleviate further damage to the eyes.
Before being placed on the transplant list, individuals must undergo a thorough evaluation to determine their suitability for a pancreas transplant. The diagnostic process involves the following assessments:
1. Comprehensive Medical Evaluation
A comprehensive medical evaluation includes a review of the patient's medical history, current health status, and the severity of their diabetes and related complications. This helps determine whether the patient is a candidate for pancreas transplantation.
2. Blood Tests
-
Blood glucose levels: Blood tests are used to assess the patient's blood sugar control and overall glycemic status.
-
Hemoglobin A1c (HbA1c): This test measures the average blood sugar levels over the past three months. High levels of HbA1c suggest poor blood sugar control, which may indicate the need for a pancreas transplant.
3. Kidney Function Tests
As many patients with type 1 diabetes also experience kidney damage (diabetic nephropathy), kidney function is assessed to determine if a combined pancreas and kidney transplant is necessary. Tests may include blood tests, urine analysis, and imaging studies to evaluate kidney health.
4. Imaging Studies
-
CT scan or MRI: Imaging tests may be used to assess the pancreas's size and structure, as well as to rule out any underlying pancreatic diseases.
-
Ultrasound: An ultrasound can be used to assess organ function and identify any complications or issues with the pancreas.
5. Psychological Evaluation
A psychological evaluation is an essential part of the transplant evaluation process, as patients must be prepared to manage the emotional, psychological, and physical demands of the transplant procedure and lifetime medication management.
Once a patient is deemed eligible for a pancreas transplant, there are several treatment options available, depending on the individual’s condition and the presence of any additional complications:
1. Pancreas Transplant Alone
In this procedure, only the pancreas is transplanted, and it is typically performed on individuals with type 1 diabetes who do not have severe kidney damage. The transplanted pancreas will restore insulin production and improve blood sugar regulation.
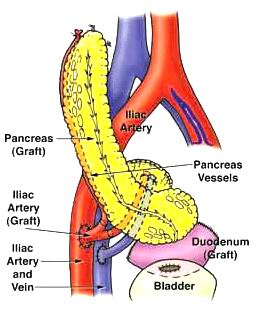
2. Combined Pancreas and Kidney Transplant
Patients with diabetic nephropathy or kidney failure may be eligible for a combined pancreas and kidney transplant. This approach addresses both the pancreas's failure to produce insulin and the kidney's loss of function, offering a two-in-one solution.
3. Living Donor Pancreas Transplant
In some cases, a living donor can provide a portion of their pancreas for transplantation. While living donor pancreas transplants are rare, they may be considered for patients with urgent needs or those who do not have a suitable deceased donor available.
4. Immunosuppressive Medications
Post-transplant, patients must take immunosuppressive medications to prevent graft rejection. These medications suppress the immune system's ability to attack the transplanted organ, but they also increase the risk of infections and other complications.
Although pancreas transplants are often a last resort for those with severe diabetes complications, there are steps that can help prevent further deterioration of pancreatic function and manage diabetes before a transplant becomes necessary:
1. Glycemic Control
-
Tight blood sugar control through insulin therapy and dietary management is critical in preventing further damage to the pancreas and related organs.
-
Regular monitoring of blood glucose levels and HbA1c can help prevent long-term complications of diabetes.
2. Regular Monitoring
Patients with advanced diabetes should undergo regular kidney function tests, eye exams, and nerve assessments to monitor for complications that could necessitate a pancreas transplant.
3. Preventing Infections
Patients with diabetes, especially those with poorly controlled blood sugar, are at a higher risk of infections. Good wound care, oral hygiene, and vaccination (flu, pneumonia) are essential to prevent infections.
While pancreas transplants have a high success rate, they can lead to certain complications:
1. Graft Rejection
Graft rejection occurs when the immune system attacks the transplanted pancreas. Symptoms include fever, pain at the transplant site, and decreased insulin production. Immunosuppressive drugs are used to prevent rejection but come with side effects.
2. Infection
Immunosuppressive medications increase the risk of infection after a transplant. Patients must follow strict guidelines to avoid infections, including avoiding contact with sick individuals and practicing good hygiene.
3. Diabetes Recurrence
In some cases, the patient’s type 1 diabetes may recur after a pancreas transplant, requiring additional insulin therapy.
4. Kidney Complications
If the pancreas transplant is combined with a kidney transplant, there is a risk of kidney rejection or graft failure, particularly if the patient’s immune system is not properly managed.
Life after a pancreas transplant requires significant lifestyle changes and ongoing care:
1. Medication Adherence
Patients must take immunosuppressive medications for the rest of their lives to prevent rejection. Managing these medications, including avoiding side effects and monitoring for complications, is crucial for long-term success.
2. Regular Follow-Up Care
After the transplant, patients will need frequent check-ups to monitor pancreatic function, kidney health, and overall immune system activity. Regular blood tests and imaging studies are necessary to ensure the transplanted pancreas is functioning properly.
3. Healthy Lifestyle
Patients should maintain a healthy diet, regular exercise, and mental health support to ensure the long-term success of the transplant and to prevent complications like obesity, high blood pressure, or cardiovascular disease.
4. Emotional Support
The process of receiving a transplant, including the recovery period, can be emotionally challenging. Psychological support and counseling can help patients adjust to the changes and manage the stress that comes with post-transplant life.
1. What is a pancreas transplant?
A pancreas transplant is a surgical procedure in which a healthy pancreas from a deceased donor is transplanted into a patient whose pancreas no longer functions properly. The pancreas is responsible for producing insulin, which helps regulate blood sugar levels. This procedure is typically performed in patients with type 1 diabetes who have severe complications or whose blood sugar cannot be adequately controlled by other treatments.
2. Why is a pancreas transplant necessary?
A pancreas transplant is necessary for patients with type 1 diabetes who have developed severe complications, such as kidney failure, or who are unable to control their blood sugar levels despite intensive treatment. The transplant can help eliminate the need for insulin injections, improve blood sugar control, and prevent or reverse the complications of diabetes, such as nerve damage, vision problems, and kidney disease.
3. What are the different types of pancreas transplants?
There are three primary types of pancreas transplants:
-
Pancreas transplant alone (PTA): In this procedure, only the pancreas is transplanted into a patient who has type 1 diabetes.
-
Simultaneous pancreas-kidney transplant (SPK): This is the most common form, in which both a pancreas and kidney are transplanted at the same time. It is often performed for patients with diabetic nephropathy (kidney failure due to diabetes).
-
Pancreas after kidney transplant (PAK): In this procedure, the pancreas is transplanted after a kidney transplant, typically in patients who received a kidney transplant for kidney failure due to diabetes.
4. How is a pancreas transplant performed?
Pancreas transplant surgery involves the following steps:
-
Anesthesia: The patient is placed under general anesthesia to ensure they are unconscious and pain-free during the procedure.
-
Incision: The surgeon makes an incision in the abdomen to access the pancreas and other organs.
-
Removal of the diseased pancreas: If the patient has an existing pancreas that is not functioning properly, it is removed.
-
Implantation of the donor pancreas: The healthy donor pancreas is transplanted into the patient’s body. The pancreas is connected to blood vessels and, if applicable, the small intestine to allow for normal digestive function.
-
Closure: The incision is closed, and the patient is taken to the intensive care unit (ICU) for monitoring.
The procedure typically takes 4 to 6 hours, and the patient will remain in the hospital for several days to weeks for recovery.
5. Is pancreas transplant surgery painful?
Pancreas transplant surgery is performed under general anesthesia, so the patient will not feel any pain during the procedure. After surgery, some discomfort, soreness, or pain around the incision site is common, but this can be managed with pain medications. Patients may also experience temporary issues like swelling or difficulty eating and drinking while recovering from the surgery.
6. How long does it take to recover from a pancreas transplant?
The recovery process varies from patient to patient, but generally:
-
Hospital stay: Patients typically stay in the hospital for about 1 to 2 weeks for monitoring and initial recovery.
-
First few weeks: Most patients can resume normal activities after 2 to 3 weeks but should avoid strenuous activity during this period.
-
Long-term recovery: Full recovery can take 3 to 6 months. Patients need to follow strict post-transplant care instructions, including taking immunosuppressive medications to prevent organ rejection and attending regular follow-up appointments to monitor pancreatic function and health.
7. What are the risks and complications of pancreas transplant surgery?
While pancreas transplant surgery can significantly improve the quality of life for many patients, there are potential risks and complications, including:
-
Rejection: The body may reject the transplanted pancreas, especially if the patient’s immune system is not properly suppressed.
-
Infections: Immunosuppressive medications increase the risk of infections.
-
Organ failure: The transplanted pancreas may not function as expected, or other organs may fail due to surgery or immunosuppressive medications.
-
Blood clots: There is a risk of blood clots forming, which could affect blood flow to the pancreas or other organs.
-
Diabetes recurrence: In some cases, diabetes may return after the transplant, particularly if there is immune system rejection or other complications.
8. How long does a pancreas transplant last?
The average lifespan of a transplanted pancreas is about 10 to 15 years, but it can vary depending on factors such as the patient’s overall health, how well the transplanted pancreas is accepted by the body, and the adherence to medication and lifestyle recommendations. The transplanted pancreas may eventually fail over time, and in some cases, patients may need additional treatments or a new transplant.
9. Will I need to take medications after a pancreas transplant?
Yes, after a pancreas transplant, patients must take immunosuppressive medications to prevent rejection of the new pancreas. These medications suppress the immune system, making it less likely to attack the transplanted organ. Patients may also need other medications to manage blood pressure, cholesterol, and prevent infections. Long-term use of immunosuppressive drugs requires regular monitoring to prevent side effects and ensure the transplant remains successful.
10. Can I lead a normal life after a pancreas transplant?
Yes, many patients are able to lead a normal, active life after a pancreas transplant, but it may take several months for the body to fully adjust to the new pancreas. Patients typically regain energy and enjoy better blood sugar control, which improves their overall quality of life. However, they must continue taking medications to prevent rejection and manage other aspects of their health, such as infections or high blood pressure. Regular follow-up care and adherence to a healthy lifestyle are essential to ensure the success of the transplant.
The other Organ Transplant Procedures are:
- Kidney Transplant
- Heart Transplantation
- Liver Transplant
- Bone Marrow Transplantation… etc
Few Major Hospitals for Pancreas Transplant are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


