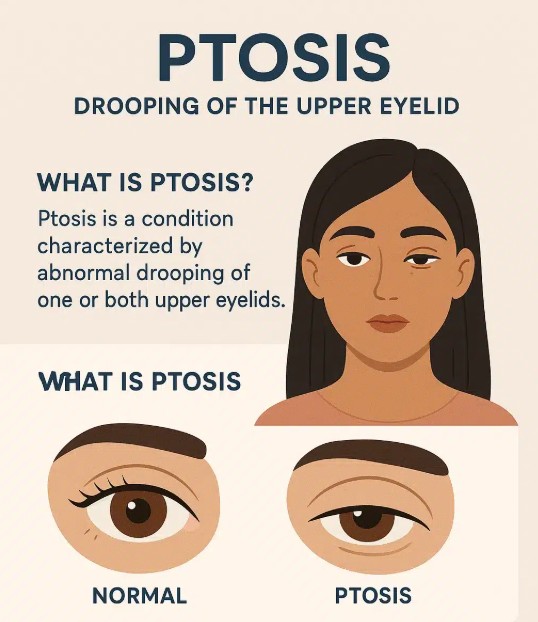
Ptosis, also known as drooping eyelid, is a condition where one or both of the upper eyelids sag or droop abnormally. This condition can affect vision if the drooping eyelid obstructs the field of vision, causing functional impairment. Ptosis can vary in severity, with some individuals experiencing mild drooping that doesn’t significantly affect their vision, while others may have more pronounced sagging that interferes with daily activities.
Ptosis occurs when the levator muscle, which is responsible for lifting the eyelid, becomes weakened or damaged. This results in the eyelid falling lower than usual, which may cause the person to raise their eyebrows or tilt their head back to compensate for the impaired vision.
Ptosis can affect individuals of all ages, from newborns (congenital ptosis) to the elderly (acquired ptosis). It can also occur as a result of nerve damage, muscle weakness, or trauma. The condition may also be associated with other eye conditions, such as dry eyes, or ocular surface disease.
Treatment for ptosis depends on the severity of the condition and the underlying cause, but it may involve surgical correction to improve the position of the eyelid, particularly if the drooping eyelid is significantly impairing vision.
The development of ptosis can be attributed to several underlying causes, ranging from congenital factors to age-related changes. Understanding these causes is essential in determining appropriate treatment options. Below are the main causes and risk factors for ptosis:
1. Age-Related Changes
One of the most common causes of ptosis in adults is the natural aging process. As people age, the muscles and tissues around the eyelid, especially the levator palpebrae superioris muscle, which lifts the eyelid, may become weakened or stretched. This leads to progressive drooping of the eyelid.
2. Congenital Ptosis
Congenital ptosis is present at birth and typically results from underdeveloped or weak eyelid muscles. Children born with congenital ptosis may experience varying degrees of eyelid drooping. If severe, it can interfere with normal visual development, which may lead to amblyopia (lazy eye). In congenital ptosis, the condition may be inherited or occur sporadically due to developmental issues during pregnancy.
3. Nerve Damage
Damage to the oculomotor nerve can result in ptosis, as this nerve controls the eyelid muscle responsible for lifting the eyelid. Horner’s syndrome, which affects the sympathetic nerves, can also lead to ptosis. Third cranial nerve palsy is another condition that can cause ptosis due to nerve dysfunction.
4. Trauma or Injury
Injuries to the eye, eyelid, or surrounding muscles may result in ptosis, especially if the levator muscle or the nerve supply to the muscle is damaged. Surgical trauma or complications from eye surgeries, such as cataract surgery, can also lead to ptosis.
5. Muscle Diseases
Certain muscle disorders such as myasthenia gravis, an autoimmune disorder that impairs neuromuscular transmission, can lead to ptosis. This condition causes weakness in voluntary muscles, including those that control the eyelids. Chronic progressive external ophthalmoplegia (CPEO) is another rare condition associated with ptosis caused by muscle degeneration.
6. Systemic Health Conditions
Ptosis can also be associated with underlying systemic conditions such as diabetes, stroke, or neurological disorders, which may affect the nerves or muscles that control the eyelids. These conditions can either directly cause ptosis or increase the risk of nerve damage that leads to the condition.
7. Tumors or Growths
In rare cases, the presence of tumors or abnormal growths in the eye socket can put pressure on the eyelid, causing it to droop. Tumors can either directly interfere with the function of the eyelid muscles or obstruct the nerve supply to those muscles.
The most obvious symptom of ptosis is the drooping of the eyelid. However, individuals with ptosis may also experience other symptoms, particularly if the condition interferes with vision. Common symptoms and signs include:
1. Drooping Eyelid
The most visible and common symptom of ptosis is the sagging or drooping of the upper eyelid. This can vary from a mild, barely noticeable droop to a severe condition where the eyelid partially or completely covers the pupil.
2. Difficulty Opening the Eyes
People with ptosis often experience difficulty opening their eyes fully. This can be due to the weakness of the eyelid muscle or the heaviness of the drooping eyelid. In some cases, individuals may feel the need to lift their eyebrow or use their fingers to open their eyelids.
3. Vision Obstruction
Severe ptosis can impair vision if the drooping eyelid obstructs the visual field, especially in the central vision. This may lead individuals to tilt their head back or use compensatory measures, such as raising the eyebrows or using their fingers to lift the eyelid to improve vision.
4. Eye Fatigue
Ptosis, especially if it affects both eyes, can lead to eye strain or fatigue. People with ptosis may experience difficulty focusing or keeping their eyes open for long periods of time, which can contribute to discomfort.
5. Double Vision (Diplopia)
In rare cases, ptosis may be associated with double vision, particularly when caused by neurological conditions like myasthenia gravis. This condition occurs when the muscles controlling eye movement are weak, leading to misalignment of the eyes.
6. Dry Eye and Irritation
If ptosis causes the eyelid to close improperly, it may lead to dry eyes or irritation due to insufficient tear production or incomplete eye protection.
A proper diagnosis of ptosis is critical in determining the most appropriate treatment options. An eye care professional, usually an ophthalmologist or optometrist, will conduct a detailed examination to assess the degree of ptosis and its underlying cause. The diagnostic process may involve the following:
1. Comprehensive Eye Exam
The ophthalmologist will perform a standard eye examination to assess visual acuity, measure eyelid position, and evaluate the degree of eyelid drooping. The doctor will also check for other potential eye conditions that may be contributing to the ptosis.
2. Measurement of Ptosis
To assess the severity of the ptosis, the doctor may measure the distance between the upper eyelid and the pupil. This will help to categorize the ptosis as mild, moderate, or severe. In some cases, photographs may be taken to track any changes in eyelid position over time.
3. Diagnostic Imaging
If the cause of ptosis is uncertain, imaging tests such as MRI or CT scans may be ordered to assess the eye socket and surrounding tissues for abnormalities, tumors, or damage to the nerve pathways.
4. Neurological and Muscle Testing
If ptosis is suspected to be related to a systemic condition such as myasthenia gravis, blood tests or electromyography (EMG) may be performed to assess the function of the neuromuscular junction. A neurological exam may also be done to evaluate the function of the oculomotor nerve and other eye-related muscles.
5. Test for Levator Muscle Function
To differentiate between congenital ptosis and acquired ptosis, the ophthalmologist may test the levator muscle’s function by observing how much the eyelid lifts when the individual attempts to open their eyes or when an eyelid is gently lifted.
Treatment for ptosis largely depends on the severity of the condition and the underlying cause. In cases where ptosis is causing visual obstruction or discomfort, treatment options may include surgical correction and non-surgical approaches:
1. Surgical Treatment (Ptosis Repair)
Surgical treatment is the most effective option for ptosis, particularly when the condition significantly affects vision or quality of life. The most common surgical procedure is levator palpebrae superioris muscle resection. This procedure involves tightening or repositioning the muscle responsible for lifting the eyelid, effectively lifting the eyelid to a more natural position.
In cases of congenital ptosis, surgery may be performed early in life to avoid the risk of amblyopia (lazy eye). The surgery can be done under local anesthesia for adults and general anesthesia for children.
There are different surgical techniques to treat ptosis, depending on the severity and underlying cause:
-
Levator advancement or resection: This involves adjusting the levator muscle to improve eyelid elevation.
-
Müller’s muscle resection: This technique is often used in patients with mild ptosis or when the levator muscle is weak.
-
Frontalis suspension: In cases where the levator muscle is too weak to function, frontalis suspension is used, where a synthetic material is used to connect the eyelid to the frontalis muscle (the forehead muscle).
2. Non-Surgical Treatment
In some cases, non-surgical treatment may be recommended for mild ptosis or when surgery is not immediately necessary. These treatments include:
-
Eyewear with eyelid lifts: Special glasses with a lid lift mechanism can temporarily raise the eyelid for people with mild ptosis.
-
Botulinum toxin (Botox) injections: Botox can be used to tighten the muscles around the eyelid and reduce the drooping in certain cases. However, this is a temporary solution and is not used for severe ptosis.
3. Treating Underlying Conditions
If ptosis is caused by an underlying muscle disease or neurological disorder, such as myasthenia gravis, treating the underlying condition can help improve ptosis symptoms. Medications, including acetylcholinesterase inhibitors, can improve neuromuscular transmission and may help lift the eyelids.
While ptosis is often caused by aging or congenital factors that cannot be prevented, managing symptoms and avoiding exacerbating factors is key to improving quality of life:
1. Regular Eye Exams
Routine eye exams can help detect ptosis early, especially for individuals who have a family history of the condition. Early intervention can prevent further progression of the condition and help manage symptoms effectively.
2. Protecting the Eyes from UV Radiation
To prevent the onset of age-related ptosis caused by sun exposure, individuals should wear sunglasses with UV protection and use hats with wide brims when spending extended periods in direct sunlight.
3. Management of Underlying Conditions
If ptosis is caused by an underlying condition, such as myasthenia gravis, diabetes, or neurological disease, managing these conditions can help control the progression of ptosis. Treatment may involve medications or other therapies to reduce symptoms.
While ptosis surgery is generally safe, there are some potential complications:
1. Infection
Infection is a risk with any surgical procedure. To reduce this risk, patients are prescribed antibiotics following surgery, and the surgical site is carefully monitored for signs of infection.
2. Scarring
Surgical scarring is a potential issue, especially if the eyelid surgery is extensive. In most cases, scarring is minimal and not noticeable, but there is a risk of visible scarring or eyelid asymmetry.
3. Overcorrection or Undercorrection
In some cases, the surgery may result in an eyelid that is too high (overcorrection) or too low (undercorrection), requiring additional surgical procedures or adjustments.
After treatment for ptosis, whether through surgery or non-surgical options, patients generally experience significant improvement in their symptoms and quality of life. Post-treatment care is essential to ensure optimal recovery:
1. Post-Operative Care
Patients will need to follow post-surgical care instructions, including the use of antibiotic eye drops, avoiding rubbing the eyes, and wearing sunglasses for protection. Avoiding excessive sunlight and practicing good hygiene will aid in the healing process.
2. Lifestyle Adjustments
In some cases, eye fatigue or dry eyes may continue after surgery. Patients may benefit from artificial tears, proper eyelid care, and limiting screen time to prevent eye strain.
3. Psychological and Emotional Impact
Ptosis can affect a person’s appearance, leading to feelings of self-consciousness or frustration. It’s important to consider emotional support and follow-up consultations to address both physical and psychological concerns.
1. What is ptosis?
Ptosis is a condition where the upper eyelid droops or sags, covering part or all of the eye. This can occur in one or both eyes and may be congenital (present at birth) or acquired (developing later in life). Ptosis can affect a person's vision by partially or fully obstructing the line of sight, depending on the severity of the condition.
2. What causes ptosis?
There are several causes of ptosis, including:
-
Age-related changes: As people age, the muscles that lift the eyelid (levator muscle) may weaken or stretch, leading to ptosis.
-
Congenital ptosis: Some people are born with ptosis due to improper development of the levator muscle or nerve issues.
-
Nerve damage: Conditions that affect the nerves controlling the eyelid muscles, such as third nerve palsy or Horner’s syndrome, can lead to ptosis.
-
Trauma or injury: Injury to the eyelid or surrounding muscles can cause ptosis.
-
Medical conditions: Diseases such as myasthenia gravis, diabetes, or neurological disorders can lead to ptosis.
3. What are the symptoms of ptosis?
The primary symptom of ptosis is the drooping of the upper eyelid. Other symptoms may include:
-
Difficulty keeping the eyelid open.
-
Excessive tiredness or strain when trying to keep the eye open.
-
Vision obstruction: In severe cases, ptosis can block the line of sight, leading to difficulty seeing, especially when reading or driving.
-
Head tilt or raised eyebrows: Some individuals with ptosis may tilt their head backward or raise their eyebrows in an effort to open their eyes wider.
4. How is ptosis diagnosed?
Ptosis is diagnosed through a thorough eye examination, which may include:
-
Physical examination: The ophthalmologist will check the severity of the eyelid droop and examine the muscles around the eye.
-
Testing for nerve function: The doctor may test the function of the nerves that control eyelid movement.
-
Assessment of the levator muscle: The ophthalmologist may check the strength and function of the levator muscle that lifts the eyelid.
-
Slit-lamp examination: This may be used to evaluate the health of the eye and the extent of ptosis.
-
Other tests: If ptosis is suspected to be due to an underlying medical condition, additional tests (such as blood tests or imaging) may be required.
5. What treatments are available for ptosis?
Treatment for ptosis depends on the severity of the condition and its underlying cause:
-
Surgery: The most common treatment for moderate to severe ptosis is surgery. The levator muscle may be tightened or repositioned to lift the eyelid. In some cases, a procedure called a frontalis sling is used to attach the eyelid to the forehead muscle, allowing the patient to lift the eyelid using their brow muscles.
-
Non-surgical options: In mild cases, ptosis can sometimes be managed with specialized glasses that have a small weight attached to the eyelid, or by using eyelid tape.
-
Treating underlying conditions: If ptosis is caused by a medical condition (like myasthenia gravis), addressing the underlying condition may improve the ptosis.
6. Is ptosis surgery safe?
Yes, ptosis surgery is generally safe and effective, with a high success rate in improving eyelid position and vision. However, as with any surgery, there are some risks, including:
-
Infection: Rare, but possible after surgery.
-
Overcorrection or undercorrection: The eyelid may be lifted too much or not enough.
-
Scarring: Some scarring can occur after surgery, though it is usually minimal and well-hidden in the natural crease of the eyelid.
-
Dry eyes: In rare cases, ptosis surgery can lead to dryness or discomfort in the eyes.
7. How long is the recovery time after ptosis surgery?
Recovery time after ptosis surgery is relatively short, although it varies by individual:
-
First week: Swelling, bruising, and mild discomfort around the eyelid are common. The patient may need to avoid bending over or engaging in strenuous activities.
-
First 2-4 weeks: Most of the swelling and bruising will subside, and the eyelid will gradually lift to its new position.
-
1-3 months: The final results of the surgery become clear, and any residual swelling will completely resolve. The patient may need to attend follow-up visits with the surgeon to ensure proper healing.
8. Can ptosis recur after surgery?
Yes, ptosis can sometimes recur after surgery, especially if the eyelid muscle weakens again or if there was incomplete correction. This can occur over time as the levator muscle may stretch or lose its strength. If ptosis recurs, further surgery or adjustments may be needed. However, recurrence is uncommon, and most patients experience long-lasting results after surgery.
9. Can ptosis affect both eyes?
Yes, ptosis can affect one or both eyes. It is more common for ptosis to affect both eyes in cases where it is caused by an underlying medical condition, such as myasthenia gravis. In some cases, one eye may be more severely affected than the other. Surgery can be performed on both eyes if necessary.
10. Is ptosis surgery covered by insurance?
In many cases, ptosis surgery is covered by insurance if it is determined to be medically necessary, such as when the drooping eyelid obstructs vision. If ptosis is purely a cosmetic concern (such as a mild droop that does not affect vision), insurance may not cover the procedure. It’s important to check with your insurance provider to determine the specific coverage and requirements for ptosis surgery.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


